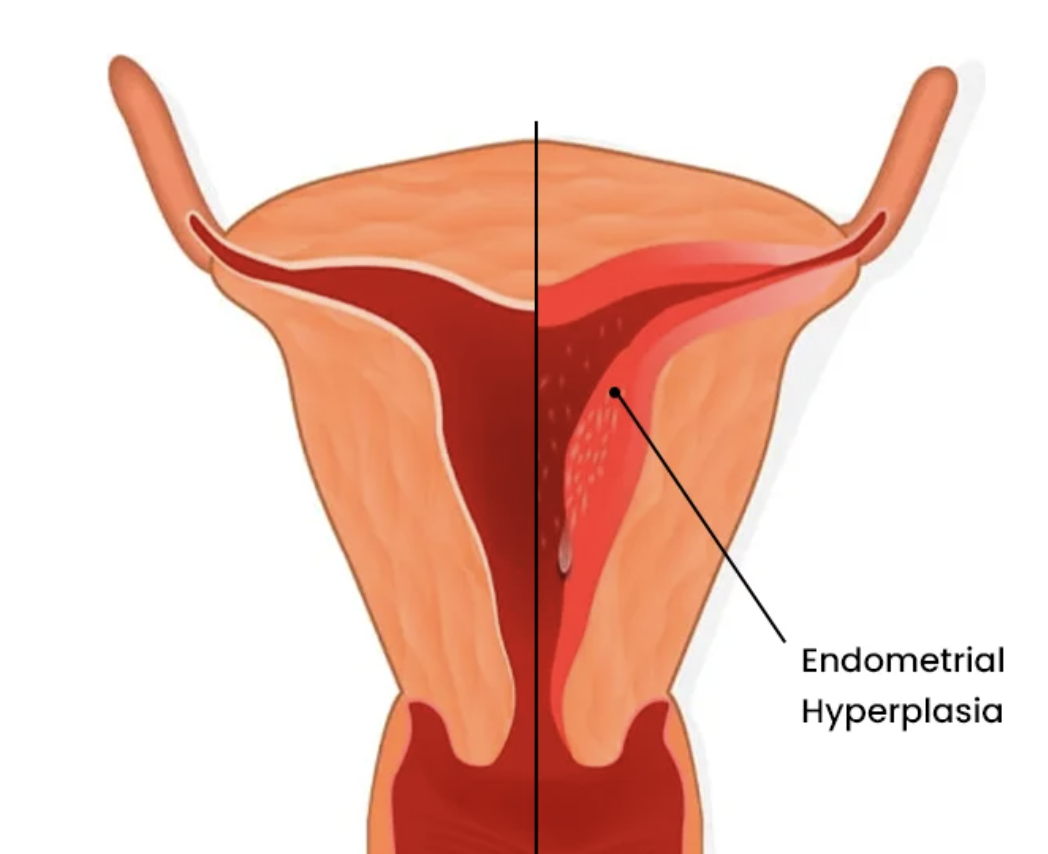
Heavy Bleeding and Endometrial Hyperplasia
What is endometrial hyperplasia?
Endometrial hyperplasia is a medical condition characterized by an abnormal increase in the number of cells in the lining of the uterus (endometrium). The endometrium is the inner lining of the uterus that thickens in preparation for a potential pregnancy during each menstrual cycle and sheds if pregnancy does not occur. Endometrial hyperplasia is when the lining of the uterus grows too thick from too much estrogen relative to progesterone. This results in an increase in gland to stroma ratio; there is more gland and less stroma when compared to normal
Causes
-
The key factor in the development of endometrial hyperplasia is an excess of circulating estrogen relative to progesterone. Estrogen promotes the growth and proliferation of endometrial cells, while progesterone helps regulate and balance this growth. When there is insufficient progesterone or an excess of estrogen, uncontrolled growth of endometrial cells can occur.
The most common reason for excess estrogen in relation to progesterone is impaired estrogen metabolism, where the body has trouble excreting estrogen properly.
-
Infrequent or absent ovulation causes low progesterone. Low progesterone levels cause an imbalance where estrogen levels are constantly high in comparison. Conditions or medications that cause anovulation may lead to estrogen dependent issues such as endometrial hyperplasia.
-
Adipose tissue (fat cells) can produce estrogen, and fat distributed around the organs is associated with higher levels of circulating estrogen. This excess estrogen can contribute to the development of endometrial hyperplasia.
-
Certain hormonal medications, such as contraceptives that prevent ovulation or estrogen replacement therapy without progesterone, may increase the risk of endometrial hyperplasia.
-
Conditions such as diabetes and polycystic ovary syndrome (PCOS) are associated with hormonal imbalances and may contribute to the development of endometrial hyperplasia.
Simple Hyperplasia: The glandular structures maintain a relatively straightforward, regular pattern without significant complexity. The endometrium contains an increased number of dilated glands.
Without Atypia: There is an increased number of cells in the endometrium, making it thicker than usual, but the cells are normal.
With Atypia: There are abnormal changes in cell structure but glandular structures are not significantly complex.
Types
Complex Hyperplasia: The glandular formations become more irregular, demonstrating a more intricate and complex pattern compared to simple hyperplasia.
Without Atypia: Increased cell growth with more complex changes, but the cells are still normal. The glands appear crowded and are surrounded by relatively scant stroma. The glandular epithelium are lined by uniform cells, which show no nuclear atypia.
With Atypia: Abnormal changes in cells that are more complex, increasing the risk of cancer. The glands appear crowded and have an irregular shape, with stratification of cells that often protrude into the lumen. Nuclei of these glands show atypia, and sometimes it is not possible to distinguish them from well-differentiated adenocarcinoma. Some pathologists call it endometrial intraepithelial neoplasia.
Symptoms
-
This is the most common symptom. It may manifest as:
Irregular menstrual bleeding and spotting
Heavy menstrual bleeding (menorrhagia)
Passing of decidual casts
Prolonged menstrual bleeding and spotting
Bleeding between periods (metrorrhagia)
Postmenopausal bleeding (bleeding after menopause)
-
Some individuals with endometrial hyperplasia experience pelvic pain or discomfort, although this is not always present.
-
People may notice changes in the regularity, duration, or intensity of their menstrual cycles.
Treatment
-
In order to address endometrial hyperplasia at the root, you must improve estrogen metabolism.
Estrogen metabolism refers to the complex process by which the body breaks down and eliminates estrogen. Estrogen is metabolized primarily in the liver, where it undergoes various chemical transformations. Two main pathways, known as the "2-hydroxylation" and "16-hydroxylation" pathways, lead to the formation of different estrogen metabolites.
The balance between these pathways is crucial, as it influences the biological effects of estrogen and its potential impact on health.
Estrogen is excreted from the liver to the gut via the bile. This is where it should be packaged to exit the body. If the gut health is balanced, it does so easily. However, certain types of bad bacteria in the gut secrete high levels of beta-glucuronidase which may contribute to increased estrogen reabsorption, leading to elevated estrogen levels in the body.
-
Progesterone naturally combats the symptoms of estrogen dominance and tells the endometrium to stop proliferating the uterine lining. Supporting progesterone with regular ovulation, herbal support, or bio-identical progesterone cream may be indicated.
-
Nutritional support that focuses on liver and gut health is imperative to support healthy estrogen metabolism. Low histamine foods may be indicated.
Histamine, a compound involved in the body's immune response, is broken down by enzymes, including diamine oxidase (DAO). Some studies suggest that elevated histamine levels may inhibit DAO activity, leading to impaired estrogen breakdown. As a result, the body may experience difficulty in efficiently metabolizing estrogen, potentially contributing to an imbalance in estrogen levels.
-
Some herbs have potential benefits for addressing impaired estrogen metabolism. Particularly herbs that address liver health (bitter herbs) gallbladder health, and gut health (mucilaginous herbs and probiotics). Other herbs are known for stimulating the menses to help shed existing lining (emmenagogues).
-
Reduce exposure to endocrine-disrupting chemicals found in certain plastics, pesticides, and household products.
Xenoestrogen are chemicals that imitate estrogen that can activate or block estrogen receptors in various tissues of the body, including the ovaries, uterus, and brain.
Xenoestrogens are serious environmental hazards that can disrupt hormonal function in all people and accumulate and persist in our fatty tissue for decades.
How To Use Charting With Endometrial Hyperplasia
Use your charts to describe the color and consistency of your blood and bleeding patterns
Use cervical fluid as a diagnostic sign to measure estrogen levels throughout the cycle
Monitor basal body temperatures to better understand if your cycles are ovulatory and if you are making adequate progesterone
Follow the healing process and changes in your charts after improving estrogen metabolism, supporting progesterone, and reducing exposure to xenoestrogens.