The Process of Ovulation
The Process of Ovulation
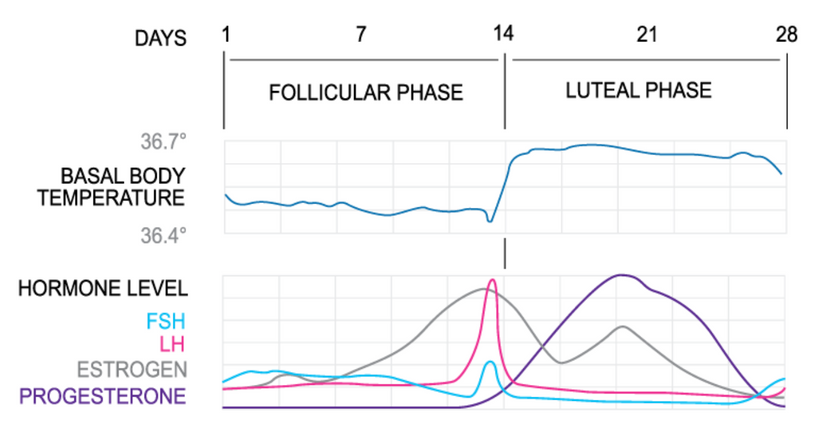
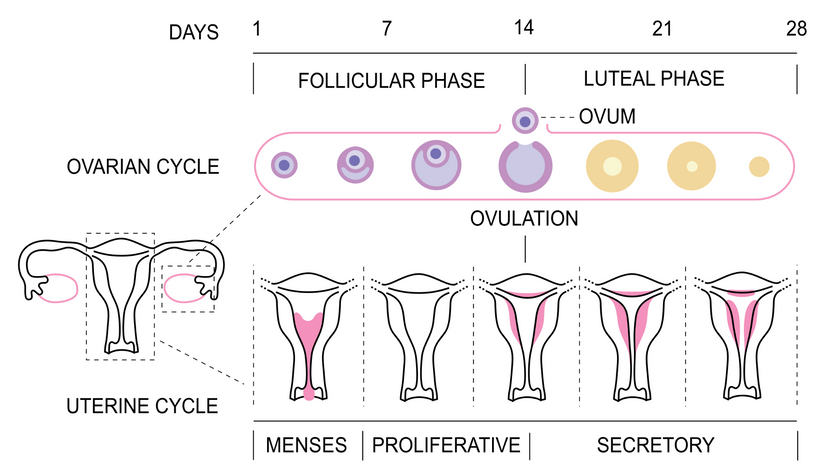
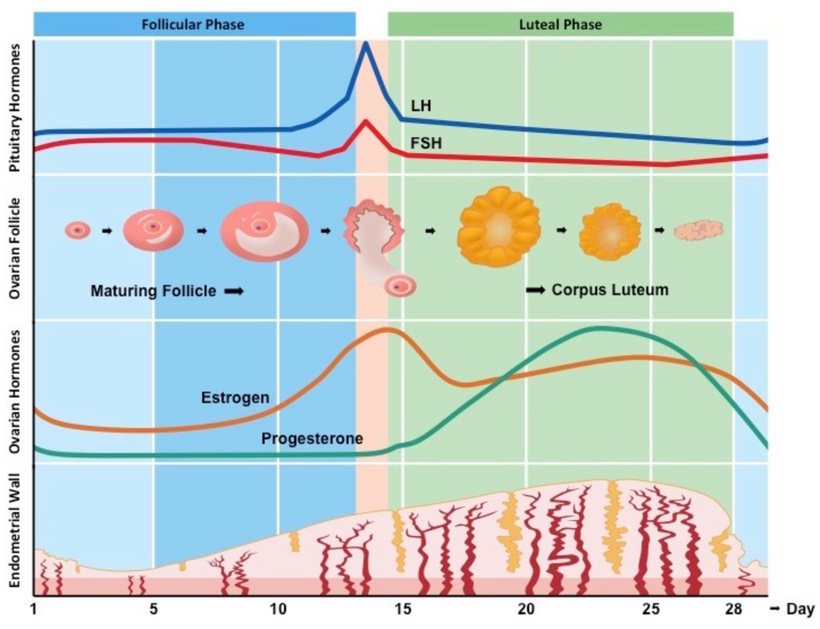
The menstrual cycle begins with the first day of a flowing menstrual bleed where estrogen levels are low. The follicular phase is the first part of the menstrual cycle, which is when the maturation of the egg-to-be occurs.
The conclusion of that process is ovulation, or the release of the egg (seen here at day 14)
Ovulation typically happens mid way through the cycle, immediately following the hormonal changes in the follicular phase. During the follicular phase, the uterus is in its proliferative phase, that is, building up endometrial (uterine) lining in preparation for ovulation. Remember that during menses, the previous cycles lining has been cleared and the process is beginning again.
In the ovaries, eggs develop in fluid sacs, which are called follicles. Follicles develop for several cycles before they are ready to release their egg, and some will never release an egg at all.
Ovulation is a physical and hormonal event at the same time.
What does this mean?
Ovulation is a physical event where the ovarian follicle ruptures & releases what is called the secondary oocyte ovarian cell. This does not happen at random, but is instead under the hormonal regulatory control of the endocrine system.
This means that the hormonal event of ovulation involves more than just the ovaries. It involves a complex feedback loop system between the brain and the reproductive system, particularly in the hypothalamus & pituitary gland.
You could even say ovulation begins in the brain.
It all begins in the hypothalamus, where gonadotropin releasing hormone (GnRH) stimulates the anterior pituitary gland to release a hormone called follicle stimulating hormone, or FSH, and thus FSH levels begin to rise. We call this interaction of the feedback loops the Hypothalamus-Pituitary-Axis, and I may refer to the HPA axis a few times here. This FSH hormone sends a message to your ovaries that we are looking to stimulate ovarian follicles, mature a follicle, and release an oocyte. Your follicles are always in various stages of development, but only a few are the ones chosen to mature as candidates for THE egg for this particular cycle.
FSH causes these selected follicles to develop special granulosa cells. These cells surround the oocytes & their most important job is to begin secreting estrogen. The pre-ovulatory follicle is the body’s primary source of estrogen, accounting for more than 90% of estrogen production in follicular phase. Here’s where we find the first positive feedback loop.
As the granulosa cells in the ovarian follicles secrete more & more estrogen, the estrogen levels peak, and this actually begins to then inhibit the secretion of Follicle stimulating hormone.
So if you think that through for a second, the brain released FSH which causes the ovarian follicles to develop & secrete estrogen, which then has a negative feedback on FSH, and FSH levels fall. This fall in FSH levels also causes smaller, less developed follicles which were competing to ovulate, to die off. About half way through the follicular phase, one follicle becomes more dominant than all the others in their stages of development.
So now FSH has fallen & estrogen is rounding off at its peak. When estrogen levels are sufficiently high - a message is sent back to the hypothalamus that we need more gonadotropin releasing hormone to stimulate the pituitary gland again, but this time to release another hormone - luteinizing hormone. By the time luteinizing hormone is released to induce ovulation, estrogen levels are already beginning to fall from their peak level.
On average, ovulation occurs 28 - 36 hours after the onset of the LH surge, or 12 hours after it reaches its peak level. When you use ovulation predictor kits - they are testing for luteinizing hormone specifically.
Luteinizing hormone stimulates enzymes secreted by the chosen follicle to degrade the follicle tissue & a hole called the stigma will form in the follicle. Ovulation begins when the secondary oocyte exits the follicle, into the abdominal cavity. Some people can even feel this rupture which is often described as ‘ovulatory pain’.
The Fallopian tubes, which are not actually attached to the ovaries, will collect the egg and send it on its way. The fimbriae, fringe cilia tissue at the end of the tubes, are activated by the sex hormones, swelling with blood & sweeping gently over the ovaries to usher the oocyte into the tube. More cilia inside the Fallopian tube move the oocyte towards the uterus.
The burst ovarian follicle has now done its job of releasing the egg. It quickly folds in on itself and transforms into a whole new temporary organ: the corpus luteum. The corpus luteum is a secreting body which produces high levels of progesterone. Progesterone is necessary to support the endometrial walls, as well as a fertilized egg. During pregnancy, the placenta eventually takes over production of progesterone from the corpus luteum. If the egg is unfertilized, the corpus luteum stops secreting progesterone, degenerates, and when progesterone levels fall, the endometrium falls, and the next menstruation occurs.
Occasionally I am asked about a ‘second ovulation’ - is this possible?
The answer is no. And this is precisely because of those feedback loops I’ve been talking about. The loops are either positive (turning hormones on) or negative (turning hormones off). When your corpus luteum releases progesterone it sends a message to the brain to suppress gonadotropin release from the pituitary gland.
So the two hormones responsible for triggering the process of ovulation: follicle stimulating hormone & luteinizing hormone - are directly inhibited by the progesterone made from the corpus luteum. Seeing that the corpus luteum can only develop post-ovulation, and releases progesterone until you bleed, the event can only occur once per cycle.
People can however, have twins through one single hormonal event of ovulation - with a little too much follicle stimulating hormone - the ovaries can release more than one egg resulting in twins, triplets, or more. There is research into how genetic factors play a role in the prevalence of fraternal twins and follicle stimulating hormone.
Because the fertile window only occurs once and results in ovulation in a healthy cycle - identifying when you are fertile can be determined in a scientific window. After ovulation, you will not be fertile again until the next cycle.
Ovulation also cannot be predicted, this is why we use diagnostic & retroactive signs in fertility awareness to determine the fertile window.
The follicular, pre ovulatory phase, is always a variable number of days. The luteal, post ovulatory phase, is always fixed. This means that anything that can affect your hormones can affect your ovulation. Environmental factors like travel, stress, exercise, and lack of sleep can affect ovulation, as well as internal factors like your diet or an underlying medical condition. A delayed ovulation, or an anovulatory cycle can happen occasionally but if you stop ovulating entirely or you consistently have trouble ovulating as seen through really long cycles, serious health conditions must be investigated.
Let’s review the process of ovulation:
The process begins in the brain
Hypothalamus tells the pituitary gland to make follicle stimulating hormone
FSH stimulates the developing ovarian follicles to secrete estrogen
Estrogen inhibits FSH + tells the hypothalamus - pituitary to release LH
LH causes the mature follicle to burst & the egg to release
The follicle inverts on itself, creating the corpus luteum, releasing progesterone
Progesterone inhibits FSH & LH - telling the HPA to stop releasing them & preventing the event from occurring again
If the egg is unfertilized, the corpus luteum degenerates, progesterone falls 2 weeks later, and the menstrual cycle concludes with the bleed.